Frozen shoulderA condition where shoulder movement becomes very limited and painful. The cause is often unknown, bu More is a condition that causes pain and stiffness in the shoulder joint. It can make it difficult to move your arm and perform everyday activities. Many people wonder what causes frozen shoulder, how to treat it, and whether or not it will go away on its own. In this article, we will answer all of your questions about what is Frozen Shoulder, its causes, symptoms, stages, treatments, and recovery tips.
What is a Frozen Shoulder?
Medically, Frozen shoulder is known as adhesive capsulitis. The shoulder joint is a ball and socket jointThe glenohumeral joint is a ball-and-socket synovial joint and is the most mobile joint in the human More, which means that the round head of your upper arm bone (humerus) fits into a shallow socket in your shoulder blade (scapula).
Frozen shoulder occurs when the connective tissue around the shoulder joint becomes stiff and inflamed. This can make it difficult to move your arm. Adhesive capsulitis often develops slowly, and symptoms can worsen over time.
The characteristic feature of frozen shoulder is complete loss of External RotationThe range of shoulder external rotation is one of the most important metrics in the field of general More.
The Three Stages of Frozen shoulder:
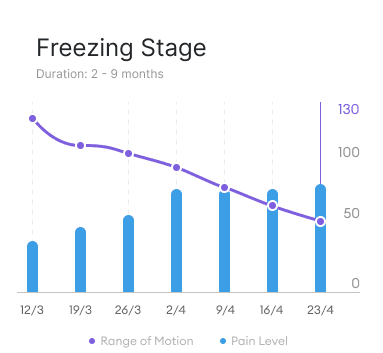
Freezing stage:
Stage I: This is the first stage of frozen shoulder and is also known as the painful phase. You may feel pain when you move your arm, and your range of motion (ROM) will start to decrease. Typically the shoulder painShoulder pain is any pain felt around in and around the shoulder joint. The shoulder is the most mob More is worse at night. The onset of pain and reduction of ROM in this stage is sometimes confused with Rotator CuffThe rotator cuff is a group of muscles and tendons that attach the shoulder blade to the upper arm b More tendinopathy. However, Rotator Cuff tendinopathy cases do not have a gradual decrease in Range of Motion, whereas adhesive capsulitis will have week-on-week reduction of shoulder range of motion.
Duration: 2-9 months
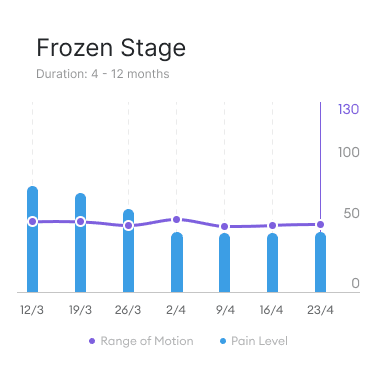
Frozen stage:
Stage II: This is the second stage of frozen shoulder, characterised by “pain and stiffness” in varying proportions. Your pain may decrease during this stage, but your range of motion will continue to decrease. In the early stages of Stage 2 of Frozen shoulder, you may primarily still be experiencing pain. The latter part of the frozen stage is characterised with more stiffness than pain.
Duration: 4-12 months
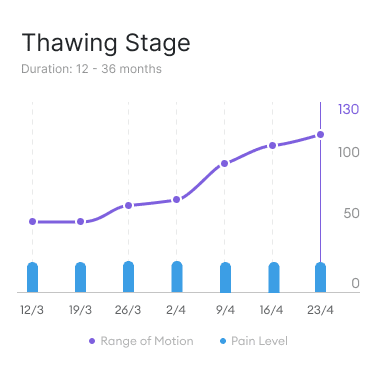
Thawing stage:
Stage III: This is the final stage of frozen shoulder. Your range of motion will start to improve, but you may still have some pain and stiffness. The gradual return of range of motion is due to reducing inflammation and fibrosis in the shoulder joint.
Duration: 12-36 months
Reference: Idiopathic Frozen Shoulder
How Long Does Frozen Shoulder Last?
Frozen shoulder typically lasts anywhere from six months to two years. However, there are some patients who show symptoms for up to four years.
Can frozen shoulder come back?
Recurrence is uncommon, however the other shoulder can become affected in up to 17% of patients within 5 years.
Most patients are able to recover their full range of motion, however some patients have reported reduced range of motion more than a decade after they had a frozen shoulder. Reduced range of motion not only increases risk of injuring your shoulder, it also impacts quality of life by restricting activities that someone used to do with full range of motion of their shoulder.
What does frozen shoulder feel like?
Frozen shoulder can cause a dull, aching pain that gets worse with movement. You may also feel stiffness and decreased range of motion in the affected shoulder. The symptoms of frozen shoulder typically develop slowly over time and worsen over the course of several months.
What is frozen shoulder pain like?
The freezing stage is associated with the highest degree of pain, lasting anywhere from six weeks to one year or more.
Frozen shoulder pain begins as a dull ache with increasing intensity over time. I felt like my shoulder joint was being jabbed with a hot metal poker. It “was on fire.” Pain radiated down my arm. Reaching up or sideways was excruciating. Dressing was next to impossible. This type of discomfort was new and took my breath away.
Janice Tovey
What Causes Frozen Shoulder?
There are two main types of frozen shoulder: primary and secondary. In both cases, frozen shoulder is caused by contracture of the glenohumeral joint; ie the tightening of the muscles, tendons, skin, and nearby tissues that causes the joints to shorten and become very stiff. Fibrous tissues also develop in the shoulder joint, creating a meshed web around the glenohumeral joint.
However the exact causes for the above mechanisms are still unclear.
Primary Frozen Shoulder
Primary frozen shoulder happens for unknown reasons and often spontaneously without an obvious preceding event . It is more common in women and people over the age of 40.
The shoulder capsule becomes inflamed. Specifically, the synovium is the connective tissue that lines the inside of the shoulder capsule. Inflammation of the synovium is called synovitis, which is often the first cause of primary adhesive capsulitis.
As well as synovitis, Primary Frozen Shoulder also shows fibrosis of the shoulder joint capsule, which the is development of fibrous connective tissues in response to injury or damage.
The main cause of primary frozen shoulder is unknown, however the initial inflammation is associated with increased collagen (the main protein building blocks in animal cells) and the presence of cytokines, which are small proteins that control the activity of other immune cells. This suggests that frozen shoulder is in part caused by auto-immune functions in the body.
Secondary Frozen Shoulder
Secondary frozen shoulder happens after a shoulder injury from over-use or from trauma of the shoulder. Damage and immobility of the shoulder can cause fibrosis and inflammation of the shoulder capsule.
What is the main cause of frozen shoulder?
You can get frozen shoulder from trauma or injury of the shoulder, or frozen shoulder can be idiopathic, arising spontaneously.
The prevalence is about 3-5% of the general population. The peak age of onset is 40-60 years of age, and women are slightly more likely to get it.
How do you get frozen shoulder?
Frozen shoulder has a prevalence of up to 20% for people with diabetes, much higher than the average. Therefore people with diabetes are more likely to get frozen shoulder.
Other co-morbid conditions for adhesive capsulitis include hyperthyroidism, hypothyroidism, hypoadrenalism, Parkinson’s disease, cardiac disease, pulmonary disease, stroke, and even unrelated surgical procedures such as cardiac surgery, cardiac catheterization, neurosurgery, and radical neck dissection.
How to Cure Frozen Shoulder
There is no cure for frozen shoulder. In most cases, the condition will simply go away by itself. However, depending on the severity of the condition and if the patient has had huge changes to their life, a range of treatments are available.
What is the best treatment for frozen shoulder?
The best treatment of frozen shoulder depends on what stage you are in, as each stage has different symptoms and pathologies.
Frozen Shoulder Treatment During Freezing Stage
The freezing stage is characterised by widespread inflammation in the joint capsule, synovium, and ligaments causing pain as the main symptom.
Treatment during the freezing stage should be to minimise pain so that you can continue with daily activities with as little discomfort as possible.
Rest and Ice
The easiest step is to rest the shoulder and apply ice packs. Application of ice can bring immediate relief to pain caused by swelling (inflammation).
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs such as ibuprofen or naproxen to help reduce pain and inflammation. NSAIDs work by blocking the production of prostaglandins, which are hormones that are involved in the process of inflammation at sites of damaged tissue in the body.
Steroids (local or oral)
Corticosteroid injections or oral steroids can be used to directly reduce inflammation in the shoulder joint. These are typically only used if NSAIDs have not worked, as they come with a range of potential side effects. Short to mid-term steroid use has shown to be effective in managing symptoms of adhesive capsulitis, however the effects were not maintained 6 weeks after stopping it.
Corticosteroids are drugs that mimic cortisol, a hormone produced by the body to temper an overreactive immune response. Corticosteroids rapidly reduce inflammation either directly or throughout the body. These can be administered orally or directly by a needle into the shoulder.
Locally injected steroids have been proven to be more effective than oral steroids for reducing pain.
Steroids are most effective during early stages of frozen shoulder- from the freezing stage to beginning part of frozen stage to control inflammation and reduce pain.
Pain-relieving Physiotherapy
The goal of pain relieving physiotherapy treatments is to reduce your discomfort and enable you can do daily activities. Pain relief may come from electrotherapy.
Electrotherapy reduces pain and increases function by increasing energy at the site of injury. Modalities include Laser, short wave diathermy and ultrasound.
Pain-relieving Physiotherapy has the best outcomes when used in conjunction with NSAIDs and/or steroids, rather than PT alone.
During periods with high pain, it is important not to do do any strenuous PT as this can increase inflammation and pain.
Remember that the goal of treatment during the freezing stage of frozen shoulder is to reduce pain, and ease normal functions of daily living, including getting better sleep.
Frozen Shoulder Treatment During Frozen Stage
Frozen stage: The loss of range of motion (ROM) is profound in this stage due to fibrosis in the joint capsule and surrounding ligaments. Treatment strategies should primarily aim towards gradually increasing and regaining range of motion with a structured mobilisation Physiotherapy program.
Hydrodilatation
Hydrodilatation (HD), also known as Distension Arthrography, can be used early in the frozen stage to break down the fibrosis structures and accelerate regaining range of motion. This treatment is the injection of saline, steroid, and local anaesthetic into the glenohumeral joint. However, not much difference is shown compared to a steroid injection into the glenohumeral joint.
NSAIDs can also be used to keep pain at bay during the frozen stage.
This is best treatment for most people with frozen shoulder. However, if mobilisation physiotherapy and Hydrodilatation has not worked for weeks to months for reducing pain and regaining range of motion, you may resort to Manipulation Under Anaesthetic (MUA) or Arthroscopic Capsular Release (ACR) treatment, both of which are discussed below.
Note that MUA and ACR are very invasive. Before making this decision, ensure that you have worked consistently with your physiotherapist and have been monitoring your shoulder range of motion. Regaining range of motion can be slow, however most people see progress over a series of weeks and months.
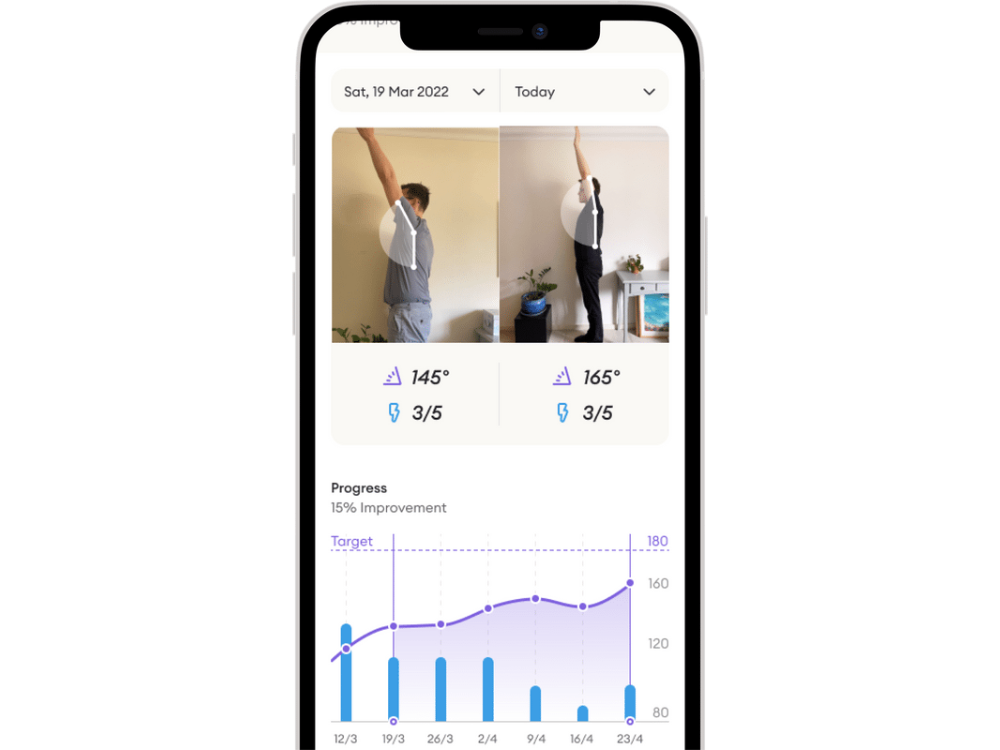
How to monitor shoulder range of motion?
You can use an app such as Reflex Health to measure your shoulder range of motion and track pain. Knowing what stage of frozen shoulder you are in is key for ensuring that you take the best course of action for your condition.
The Reflex Health App is easy to use and provides accurate range of motion measurements for your shoulder. You can simply download the app from the AppStore, create an account you will be guided through the exercises and view your measured ROM on the screen. It uses your front-facing camera and you can do a full assessment in 4 minutes from home.
Frozen Shoulder Treatment During Thawing Phase
In the final phase of frozen shoulder, pain will be minimal or non-existent with gradual increase of range of motion over the last few weeks. At this stage, surgery treatments are no longer needed.
Physiotherapy is the main treatment- from mobilisation to increasing strength in your shoulder.
How to fix frozen shoulder
If the above conservative treatments of frozen shoulder, the following operative procedures are used to fix the shoulders. By breaking or removing the connective tissues in the shoulder joint, range of motion is restored.
Surgical Treatments
In severe cases of Frozen Shoulder, surgery may be necessary to release the tightened tissue around the shoulder joint. Surgery should only be considered if after 6-9 months of the conservative treatment above has not been successful in relieving the symptoms.
The main surgery options for primary frozen shoulder are Manipulation Under Anaesthesia (MUA) and Arthroscopic Capsular Release (ACR).
Manipulation Under Anaesthesia (MUA)
MUA for frozen shoulder is a method of moving the arm through ranges of motion under anaesthesia. The fibrous shoulder capsule prevents ROM of the shoulder, and forcibly moving the shoulder joint through the range of motion breaks these fibres.
MUA is an effective way of treating primary adhesive capsulitis in the frozen stage (Stage 2), where external rotation is less than 50% of the “good arm”. MUA should not be performed for patients with secondary frozen shoulder. If you have secondary frozen shoulder, you should opt for Arthroscopic Capsular Release.
How Manipulation Under Anaesthesia is Performed
MUA does not require cutting into the body or other specialist equipment. Under anaesthesia, the patient’s shoulder is gently moved through the normal ranges of motion of the shoulder:
- FlexionIs an upgoing movement from the front side or the sagittal plane facilitated by the pectorals, anter More
- AbductionIs a sideways upgoing movement in the frontal plane brought about by the supraspinatus and the mid More
- Internal & external rotation, with the arm at 90º abduction
- External rotation with arm close to the chest
- Cross-body adduction


These movements will break the fibrous web that has grown in the shoulder complex. The breaking of fibres can often be felt or heard by the surgeons. During the procedure, the surgeons will not push against and excessive resistance from the frozen shoulder. Instead, they will move to the next exercise in the sequence. The movements are then repeated to ensure all ranges of motion has been acquired.
Often, surgeons will inject local anaesthetic and/or steroid injections, to reduce post-operative pain. However there is not much evidence to show if this is necessary.
MUA has shown to be effective with improvements lasting long term for the patients. The timing of the treatment does not impact results, so you don’t need to rush to make a decision to get it done.
What are the risks of Manipulation Under Anaesthesia?
The data for MUA shows a complication rate of 0.4%. The range of motion of flexion and abduction respond very well to MUA, however there may still be reduced ROM in external and internal rotation. The lack of recovered ROM is due to surgeons being careful when performing external internal rotation movements.
During the procedure, the surgeons will support your scapula and shoulder joint appropriately for each movement.
Although rare, some complications have been reported for MUA, typically when the surgeons push to reach terminal range of motion.
MUA for patients with diabetes
Patients with Diabetes achieve the same benefits of regaining shoulder range of motion after MUA. However 36% of diabetic patients required a repeat procedure, compared to 15% of non-diabetic patients.
Arthroscopic Capsular Release (ACR)
Arthroscopic Capsular Release has become the preferred treatment for Frozen Shoulder compared to MUA. However there is no strong evidence to suggest that it is better.
“Arthroscopy” is the procedure of inserting a narrow tube connected to a fibre optic cable into the shoulder joint.
What is Arthroscopic Capsular Release (ACR)?
The capsule is a layer of tissue that surrounds the shoulder joint. The Frozen Shoulder will cause the shoulder capsule to thicken and contract, which then limits movement at the shoulder.
Arthroscopic Capsular Release involves cutting some of the fibrous tissue around the capsule to allow for more movement in your shoulder. This is done by making several small incisions (portals) around the shoulder. Fibre-optic camera is inserted into one portal and surgical instruments are inserted into other portals. The surgeon will look at the shoulder through the camera while removing tissue to release the capsule. A radio frequency device (RFD) is used to remove the tissues using heat. The tissues thickness can be 4 mm or up to 7 mm thick.
Arthroscopic Capsular Release (Video)
The Arthroscope is typically 2.9 mm wide and inserted through the posterior portal, which is located 2 cm below and 2 cm towards the centre of your body from the acromion. You can feel your acromion with your opposite hand reaching across your chest to your shoulder, it is the bony tip of your shoulder blade (scapula). Reaching a finger over the acromion, you can feel where the posterior portal would be.
Arthroscopic Capsular Release is done as an outpatient procedure, which means you will not need to stay overnight in the hospital. The procedure typically takes 30-60 minutes. The surgeon will work quickly to reduce inflammation of the shoulder joint.
MUA after ACR
After the procedure, the surgeon will perform Manipulation Under Anaesthetic of the shoulder, as described above. This ensures that full range of motion of the shoulder has been regained
Physiotherapy after Arthroscopic Capsular Release
Aggressive physiotherapy is recommended after ACR, nay, necessary, with no restrictions on range of movement of the shoulder. Before signing up for ACR, you must buy into the treatment. The treatment will only be effective if it is followed suitable physiotherapy as prescribed by your medical professionals.
Arthroscopic Capsular Release for Diabetics
Patients with Diabetes have reported clear benefits of ACR, however there are reports of reduced ROM and higher pain compared to non-diabetic patients after ACR.
Post-Operation Care after MUA or ACR
Suitable pain control is required for 2-3 weeks using NSAIDs and Ice packs is necessary after ACR and MUA treatments.
Physiotherapy after Surgery
A structured Physiotherapy programme is essential for the next 4-6 months after surgery. The goal of physiotherapy is to maintain the regained range of motion from the procedures.
The physiotherapy programme should consist of early passive and active-assisted Range of Motion exercises with scapula stabilisation in the first stage.
This is followed by strengthening exercises for rotator cuff, scapular muscles, and core rehabilitationRehabilitation is the process of helping a person regain strength and function after an injury. This More.
MUA vs. ACR
Before starting an invasive procedure to cure frozen shoulder, patients must follow the conservative treatments effectively for 6-9 months. Only if these treatments have not produced effective results, then invasive procedures can be explored.
There is no evidence proving the superiority of ACR or MUA over the other. MUA is the most cost-effective way to treating severe cases of frozen shoulder. A study has shown that complication rates for both MUA and ACR are 0.05%.
Conclusion
Frozen shoulder is a debilitating condition that can be treated with various methods, both conservative and invasive. Conservative treatments include managing pain and following advised physiotherapy programmes best suited to the current stage of frozen shoulder.
Arthroscopic Capsular Release (ACR) and Manipulation Under Anaesthetic (MUA) are two of the most invasive procedures for frozen shoulder, but should only be considered after 6-9 months after the onset of adhesive capsulitis and enthusiastic participation in conservative treatments.
Take control of your shoulder recovery with Reflex Health
With Reflex Health monitor your shoulder range of motion and shoulder pain over time. Users say “It would be like going on a diet without tracking your weight loss.” Take control today by downloading the Reflex Health App.


